As they have for eons, most doctor’s visits begin with measurements that are stored in patient records: weight, height, pulse, blood pressure, temperature. Those numbers don’t give a complete medical picture, says Debra Leonard, M.D., Ph.D., but are still measured and recorded.
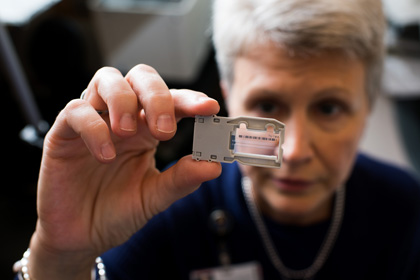
Debra Leonard, M.D., Ph.D., chair of Pathology and Laboratory Medicine at the Larner College of Medicine at the University of Vermont
As they have for eons, most doctor’s visits begin with measurements that are stored in patient records: weight, height, pulse, blood pressure, temperature. Those numbers don’t give a complete medical picture, says Debra Leonard, M.D., Ph.D., but are still measured and recorded. Although a patient’s genome also won’t provide a complete medical picture, it will be “foundational medical information” that allows physicians to fine tune treatments, and patients to make informed medical and lifestyle choices, says Leonard, chair of the Department of Pathology and Laboratory Medicine at the Larner College of Medicine at the University of Vermont. Once a billion-dollar quest, today genomic sequencing is an accessible arrow in the healthcare quiver — in many cases, it’s even covered by insurers. And while it may seem like the kind of healthcare perk that’s found only at major urban medical centers, it’s not. In fact, Leonard’s vision is that within a decade, every patient who is treated at the UVM Medical Center will have had his or her genome sequenced. With the opening of a brand new Genomic Medicine Laboratory in January 2017, she’s well on her way toward that goal.
“Pathology and Laboratory Medicine results represent approximately 80 percent of the data in the electronic health record, and we drive approximately 70 percent of medical decisions. So if we do what we do better, then we can improve care for our patients,” says Leonard. “The clinical aims of the Affordable Care Act and the Medicare Shared Savings program are improving patient experience, the cost effectiveness of care, and population health management and outcomes. And that’s the promise of genomics.”
Leonard arrived at the Medical Center in April 2013. The establishment of a genomic medicine program and construction of the $2.5 million Genomic Medicine Laboratory wouldn’t have happened without unequivocal support from Frederick Morin, M.D., dean of the Larner College of Medicine and John Brumsted, M.D., CEO of the UVM Medical Center.
“I have never worked at a place that is so collaborative,” says Leonard, who has experienced the opening of four labs in her 25-year career in molecular pathology. “This is absolutely the best lab I’ve ever had and ever seen,” she says of the new genomic medicine facility.
Eventually, she wants all patients in the UVM Health Network to have their genome screened for more than 1,000 diseases and conditions.
“If we understand the genomic variants an individual has, we can better understand their disease risks and catch diseases earlier, or know we need to screen for them before they’re happening, or suggest preventive strategies,” says Leonard. “If the patient doesn’t have the colon cancer risk variant, you could return them to the population screening level of colonoscopy every five years instead of colonoscopy every year. More expensive therapies could be targeted to those people predicted to respond. I’d been participating in both the genomic medicine and the healthcare reform conversations nationally for years, but nobody was listening about the relationship between the two issues. I came to UVM and people listened.”
For now, the spotlight is on cancer, specifically solid tumors, which are the focus of a 29-gene panel they began in February 2016.
“Sequencing is a game changer — it opens so many possibilities,” says Claire Verschraegen, M.D., M.S., deputy director of the UVM Cancer Center. “This is the dawn of oncology, where we’re starting to understand which are the most effective treatments in a certain number of patients. We’re also realizing that what we used to call ’lung cancer’ is 10 or 12 different diseases, and each of them needs a personalized type of treatment.” Already, says Verschraegen, cancer patients in whom targetable mutations were found are now heading toward complete remission; without the precision treatment made possible by sequencing, they otherwise likely would not have survived. The testing also translates to financial savings, since one gene panel can assess the effectiveness of multiple treatments, eliminating the old practice of analyzing each drug’s target one at a time.
“In two to three years we predict that we’ll be starting to do genomes for groups of patients with specific diseases, including cardiovascular disease and neurologic or neuromuscular disease,” says Leonard. Sequencing will also be a tool for children who have what appears to be an inherited disease, but for whom standard gene testing hasn’t provided answers. “If you sequence both parents and the child you can look for a recessively inherited disease or a new genetic change in the child. It limits the number of variants that you’re looking at to see if they correlate with the disease symptoms the child has. In 25 to 40 percent of kids, you can identify a variant that explains their disease process. So you have a diagnosis. Sometimes there’s treatment and sometimes there isn’t, but at least you stop the diagnostic odyssey for the child and the family,” she says.
Leonard — who counts “Multiplicity” and “Gattaca” among her favorite movies — walks the walk: she and her husband gave each other the gift of genome sequencing for Christmas.
“A lot of people say, ‘Aren’t you scared what the genome will tell you? There’s so many things in there we don’t know what to do with,’” says Leonard. “Well, yeah. But there’s a lot we do know what to do with now, and we’ll learn more about the stuff that we don’t know.” But she acknowledges that clinical genome sequencing carries a social responsibility and raises ethical questions. To that end, 73 UVM staff and faculty members underwent genome sequencing earlier this year to raise awareness about plans for clinical genome sequencing at UVM. A post-sequence survey looked at the experience overall, and Leonard and her team will follow up with the ten who signed up to participate but dropped out before sequencing to better understand their concerns.
Though genomic sequencing is not new to the College of Medicine, its clinical application is, a fact that has been acknowledged well beyond the state’s borders.
“Debra is bringing genome sequencing into clinical medicine in ways that should make UVM a model system for others to emulate,” says Geoffrey Ginsburg, M.D., Ph.D., co-chair of the National Academies of Science, Engineering and Medicine (NASEM) Roundtable on Genomics and Precision Medicine, of which Leonard is a member representing the College of American Pathologists. Adam Berger, Ph.D., a former NASEM Roundtable staffer who is now a senior fellow in the U.S. Department of Health and Human Services, says, “At the Roundtable, we were really looking at how you build a genomic medicine program — how to integrate genetics and genomics into clinical practice. Debra is out there actually doing it. It’s a great effort to be initiated and she’s the perfect leader.”
It’s safe to say it wouldn’t be happening for a long time at the College of Medicine — if ever — if Leonard had listened to her undergraduate advisor, who told her she was not cut out for medical school, although she’d planned on being a doctor from the age of 14. Like so many who choose medicine, she says she always wanted “to help people,” without grasping what that might look like: “I didn’t really understand what ’help people’ would mean over the long term of my career, because I thought it was help sick people.” Lacking the mentoring she now recognizes she needed, Leonard revised her plan to be a doctor, and after college graduation took a job as a technician at the Eaton- Peabody Laboratory at Massachusetts Eye and Ear Infirmary, assisting researchers from Harvard, MIT, and Massachusetts General Hospital.
With her college advisor’s comment echoing in her head, Leonard then went to New York to start Columbia’s two-year BSN program with an eye to becoming a nurse practitioner. Newly married to an NYU graduate student, she also needed to find a job, which she did by knocking repeatedly on the door of an auditory physiology research lab at Columbia where Shyam Khanna, Ph.D., was working. She helped conduct research that would be published, but perhaps more importantly, Khanna told her right out of the gate that she belonged in medical school. It was a message she had trained herself to ignore, but when another colleague asked if she’d ever considered an M.D./PhD program she reconsidered. She was accepted into the NYU Medical Scientist Training Program and earned a Ph.D. in molecular biology in addition to her M.D. Even then, she says, she stuck her fingers in her ears every time the head of the program said pathology was the only place for dual-doctoral degrees, continuing to believe she wanted to be Marcus Welby, the quintessential family practice physician. But her next evolution, to mother — she had one son in the middle of her Ph.D. program and another in the first year of her residency — forced her to acknowledge that the 100-hour or more work weeks (there were no work hour limits for residents at that time) that would be part of an internal medicine residency and fellowship, coupled with the demands of parenthood, were more of a juggle than she was prepared to undertake.
Another take-away from that period that Leonard brings to her role as chief is the importance of a life beyond medicine: “We’re a family-friendly department because there’s no good time to have kids. Whenever someone decides to have kids, it’s fine with me — my only rule is I have to hold the baby.”
As Leonard was looking for her first faculty position, it was an exciting time in pathology: polymerase chain reaction had just been discovered and molecular pathology and diagnostics were being developed. Leonard accepted a position at Case Western Reserve, where she was the lone molecular pathologist and tasked with the responsibility of establishing a clinical molecular laboratory, before moving on to the University of Pennsylvania, where she took over a larger clinical laboratory. After almost a decade there, Leonard went to Weill Cornell Medical College, where she served as vice chair of laboratory medicine and oversaw the creation of a molecular pathology laboratory while also serving as chief diversity officer for the medical college. All the while, on the heels of the Human Genome Project, next-generation sequencing that would make possible the sequencing of a patient’s genome was beginning to look like a clinical reality.
“We weren’t sure at that point whether you would even want to ever do a genome sequence on a patient,” says Leonard, “but there were a lot of diseases where doing large segments of the genome would be much more cost effective than testing one gene at a time as separate tests.” Nextgen sequencing was being put into play in clinical laboratories, but only at large universities. Leonard, who had been part of a national discussion about ACOs and the future of healthcare reform, saw an opportunity for genomics to play a role in patient care in Vermont, which was then tackling single-payer healthcare. Yet for the UVM Medical Center, with its relatively small catchment of less than a million patients, classic molecular testing that looked at a mutation in a single gene wasn’t feasible. Fortunately, gene panels using next-gen sequencing offered an alternative, and today, with a 29-gene solid cancer panel now in use, Leonard and her colleagues will next develop multi-gene panel tests for blood cancers and inherited cancer risk, followed by pharmacogenomics. The final step will be entire genomes.
The new laboratory, at 5,000 square feet, encompasses three individually pressurized laboratory rooms. Niki Sidiropoulos, M.D., leads the Genomic Medicine Laboratory, working with Leonard and two other molecular pathologists, technical specialists, medical technologists, genetic counselors, and a pre-authorization staff member.
“We’re not only developing the tests, but working with the healthcare team to integrate our genomic tests into care pathways,” says Sidiropoulos. “Everyone on this team is dedicated to building the best possible service. We view ourselves as offering a quality service, and not just testing” — though it’s worth noting the team has been commended by outside sequencing companies for the quality of its data — attributing much of that to Leonard’s leadership. “To be a young faculty member and have that kind of inspiration in your chair — she’s a colleague — is just truly remarkable,” especially in a relatively new field, she says. Mentoring has long been important to Leonard. She especially watches out for those who aren’t familiar with the mechanics of higher education. “I learned about academia on my own. I don’t think it should have to be that hard for people who want an academic medical career with a goal of helping others,” she says. She directed the residency training program at Weill Cornell, and maintains a philosophy that “once you’re my mentee, you’re my mentee for life."
Leonard is busy on a national level, too. She’s proud of her work to fight gene patents and served as an expert witness in the ACLU’s lawsuit against Myriad Genetics. That case went all the way to the Supreme Court, which ruled that genes are products of nature and therefore can’t be patented. She has been a member of the Association for Molecular Pathology (AMP) since it formed in 1992, and served as president and chair of its professional relations committee, through which she worked with the U.S. Food and Drug Administration on regulatory oversight of molecular testing. She was on the molecular pathology committee and the council on government and professional affairs for the College of American Pathologists (CAP) and chair of its personalized healthcare committee. She’s currently on the external scientific advisory committee for ClinGen, an initiative by NIH’s National Human Genome Research Institute to curate information about genomics. She served on the HHS Secretary’s Advisory Committee on Genetics, Health and Society, which facilitated the passage of the Genetic Information Nondiscrimination Act (GINA). She’s a leader in a field that doesn’t have a lot of women in positions of power. One such woman, Lydia Pleotis Howell, M.D., says only about 19 percent of the pathology chairs in the United States are women. Howell, chair of pathology and laboratory medicine herself at the UC Davis Health System, named Leonard her department’s Benjamin Highman Lecturer in 2015; after giving the Highman address, Leonard spoke at a session of Women in Medicine and Health Science. It was, says Howell, inspirational.
“You look at someone’s CV and it looks so easy, but you have no idea the twists and turns and challenges, but she was open and candid and personal,” says Howell. “Debra is a great role model for women leaders, and really cares about developing more women professionally.”
Within her own department, Leonard has upended the notion of what it means to be chair. Leonard had observed many chairs who were unhappy in the role and stressed by administrative expectations, but she is having a blast in her leadership role. Leonard realized that a chair should be “outward facing,” helping to steer leadership and strategy for the entire institution, as well as leading the department. She initiated a seven-month strategic planning process that included surveying the 450 department members on their professional values. She designed her executive council composed of department division chiefs, vice chairs, and business administrators that meets weekly to implement the strategic plan with 10 objectives, including the idea of “one department” to ensure that the common values are emphasized and recognized.
Leonard explains, “I didn’t think that I could hold people accountable for their behavior until I told them how we are to behave as a department. The culture of the department is really important to me.”
During meetings, executive council members and others are encouraged to fiddle with the Legos and wood Transformer toys Leonard keeps in a bucket alongside a bowl of Lake Champlain chocolate squares. Leonard, an avowed chocoholic, maintains a larger stash of gifted chocolate in her desk. It’s been something of a theme since her first academic position, where the chair, Leonard Jarrett, M.D., also a chocolate connoisseur, teased her about starting the job on April Fool’s Day. On her first work anniversary she gave him a box of chocolates — with nothing inside (she generously delivered the contents to him on April 2nd).
“About two weeks later I got a letter from him that I still have,” she laughs. “It says, ‘Dear Dr. Leonard, I am sorely disappointed in your progress to date that you have not identified the chocolate addiction gene.’”
Stand by.