
July 22, 2020 | Volume II, Issue 14
Equity & Inclusion Excellence Certificate Cohort Completes Course, Launches Capstone Projects
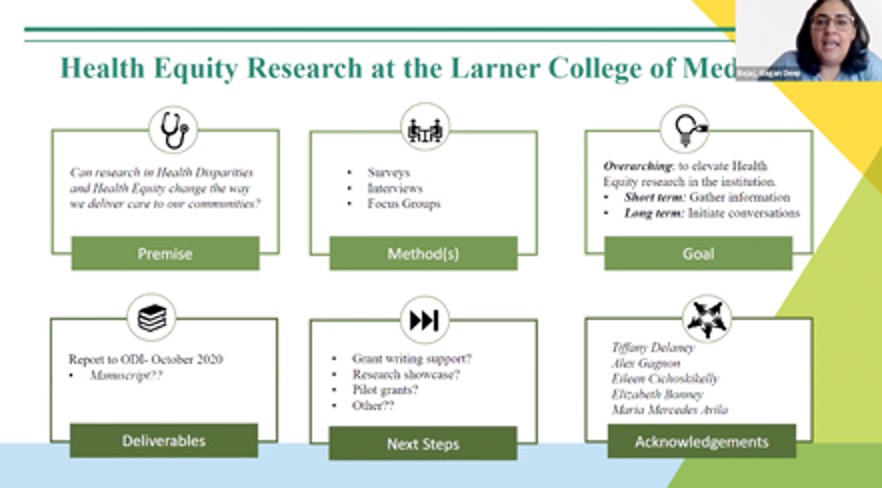
The Office of Diversity, Equity & Inclusion (ODEI) celebrated the completion of the inaugural cohort for its "Finding Our Common Ground Equity & Inclusive Excellence" certificate series with an online graduation and capstone project presentation on June 29. Associate Dean for Diversity, Equity & Inclusion Margaret Tandoh, M.D., and Larner College of Medicine Dean Rick Page, M.D., presented welcome remarks, followed by an overview of the program by ODEI Director Tiffany Delaney, M.A.Ed., who developed the 10-month program with support from ODEI staff and the Dean’s Advisory Committee on Diversity, Equity & Inclusion staff subcommittee. Certificate participants Ramsey Herrington, M.D., division chief of emergency medicine and assistant professor of surgery, and Gagan Bajaj, Ph.D., grant specialist in the Department of Medicine, provided reflections on their respective experiences in the certificate program.
The course curriculum, which focuses on developing equity and cultural humility skills in an interactive and dynamic setting, “reflects the Larner College of Medicine's highest belief of professionalism,” said Ms. Delaney.
The 20 members of the first cohort included both faculty and staff. At the completion of the program, participants were charged with identifying capstone projects to carry out in the months following graduation. Representatives from each project group presented on their project during the online event.
See the event program for a list of capstone projects.
Learn more about the Finding Our Common Ground certificate program.
Pictured above: Dr. Bajaj presents her capstone project via Zoom during the online graduation ceremony.
New Telemedicine Course: From Bed-side to Web-side
In just a few short months, the COVID-19 pandemic has spurred countless innovations in medical education, especially at the Larner College of Medicine. Among them, a new course for third- and fourth-year medical students developed by Cate Nicholas, Ed.D., M.S. P.A., education director for the UVM Clinical Simulation Laboratory, specifically geared toward the type of care many patients have become accustomed to during the new normal of social distancing–telehealth.
Drs. Nicholas and Everett have presented the course to various programs and departments at the UVM Medical Center, at several virtual conferences, to the AAMC Directors of Clinical Skills Group, and to the American Medical Association. In the coming months, they hope to work with the UVM Medical Center to formally include students in telemedicine patient visits.
Pictured above: Class of 2022 medical student Kalin Gregory-Davis (left) participates in a practice telehealth visit with Clinical Simulation Laboratory Standardized Patient Educator Bob Bolyard (right).
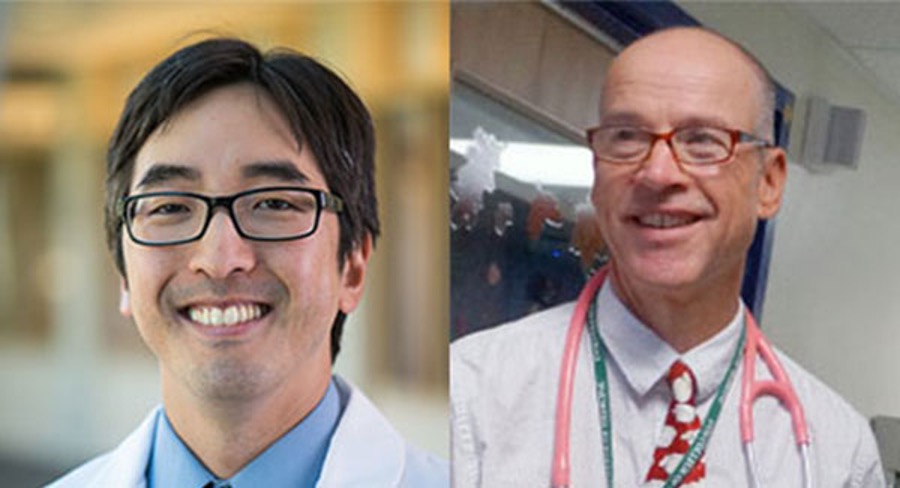
Lee and Raszka Commentary Addressing COVID-19 Transmission in Kids, Safe Reopening of Schools
A commentary published in Pediatrics by Assistant Professor of Pediatrics Benjamin Lee, M.D., and Professor of Pediatrics William V. Raszka, M.D., concludes that children infrequently transmit COVID-19 to each other or to adults and that many schools, provided they follow appropriate social distancing guidelines and take into account rates of transmission in their community, can and should reopen in the fall. Titled “COVID-19 Transmission and Children: The Child Is Not to Blame,” the commentary references a new study from the University of Geneva (Switzerland) in Pediatrics, and four other recent studies, two from China, and one each from France and New South Wales, that examine COVID-19 transmission by and among children.
“The data are striking,” said Dr. Raszka. “The key takeaway is that children are not driving the pandemic. After six months, we have a wealth of accumulating data showing that children are less likely to become infected and seem less infectious; it is congregating adults who aren’t following safety protocols who are responsible for driving the upward curve.”
Additional support for the notion that children are not significant vectors of the disease comes from mathematical modeling, Drs. Lee and Raszka said. Models show that community-wide social distancing and widespread adoption of facial cloth coverings are far better strategies for curtailing disease spread, and that closing schools adds little. The fact that schools have reopened in many Western European countries and in Japan without seeing a rise in community transmissions bears out the accuracy of the modeling.
Drs. Lee and Raszka believe that reopening schools in a safe manner this fall is important for the healthy development of children. “By doing so, we could minimize the potentially profound adverse social, developmental, and health costs that our children will continue to suffer until an effective treatment or vaccine can be developed and distributed, or failing that, until we reach herd immunity,” they concluded in their paper.
Read more about the commentary and related study findings.
Link to a list of national media coverage of Drs. Lee and Raszka’s commentary.
Pictured above: Drs. Lee (left) and Raszka.

Avila Discusses Health & Racial Disparities in
COVID-19
“My research shows that the biggest knowledge gaps for providers relate to
– Excerpted from a UVM Larner College of Medicine blog post, titled “Health and Racial Disparities in COVID-19,” by Maria Mercedes Avila, Ph.D., associate professor of pediatrics, director of Vermont Leadership Education in Neurodevelopmental Disabilities (LEND) and health equity liaison in the College’s Office of Diversity, Equity & Inclusion. Dr. Avila was recently named to the Vermont Racial Equity Task Force commissioned by Governor Phil Scott. Out of over 160 applications, she was one of three community members chosen for her “extensive experience in equity work, community advocacy, and addressing the nuances of intersectionality for various groups that have been historically marginalized.”
TEXT ONLY VERSION: Join the Social Justice Coalition Book Club and participate in productive dialogue and critical thinking about advocating for a more equitable and anti-racist world. Email sjclcom@gmail.com to join.
Video Series Seeks to Inform Public About Science Behind COVID-19
The Larner College of Medicine Graduate Student Council has developed a video series to help the public understand the science behind the COVID-19 pandemic. The first video in the series, called “COVID-19 Explained: Understanding the Pandemic with Basic Science,” developed by Cellular, Molecular, and Biomedical Sciences doctoral candidates J.J. Bivona and Marcus Weinman, explains how scientists use PCR tests to determine infection with the SARS-CoV-2 virus.
Accolades & Appointments


Matthew Albaugh, Ph.D., assistant professor of psychiatry, received a four-year, $750,000 K award from the National Institutes of Health. The project will utilize data from the Adolescent Brain and Cognitive Development (ABCD) study to develop risk algorithms for anxiety and depression in adolescents and will also involve training at Harvard Medical School and McGill University. Co-investigators include Rex Forehand, Ph.D., professor of psychological science; Peter Dodds, Ph.D., professor of mathematics and statistics; Hugh Garavan, Ph.D.,professor of psychiatry; Alexandra Potter, Ph.D., associate professor of psychiatry; Alan Evans, Ph.D., professor of neurology and neurosurgery, psychiatry and biomedical engineering at McGill University; Nikos Makris, M.D., Ph.D., associate professor of psychiatry and neurology at Harvard Medical School; and James Hudziak, M.D., Achenbach chair in developmental psychopathology and professor of psychiatry.

CITATION HIGHLIGHTS
Moulton H, Moulton B, Lahey T, Elwyn G. Can Consent to Participate in Clinical Research Involve Shared Decision Making? AMA J Ethics. 2020 May 1;22(5):E365-371. doi: 10.1001/amajethics.2020.365. PMID: 32449651
Lahey T, Elwyn G. Sliding-Scale Shared Decision Making for Patients With Reduced Capacity. AMA J Ethics. 2020 May 1;22(5):E358-364. doi: 10.1001/amajethics.2020.358. PMID: 32449650
Lahey T. Drug Testing Is No Substitute for Honesty or Addiction Risk Reduction. Am J Bioeth. 2020 Jan;20(1):75-77. doi: 10.1080/15265161.2019.1689309. PMID: 31910133
Lahey T, Nelson W. A Dashboard to Improve the Alignment of Healthcare Organization Decisionmaking to Core Values and Mission Statement. Camb Q Healthc Ethics. 2020 Jan;29(1):156-162. doi: 10.1017/S0963180119000884. PMID: 31858947
Pantoni MM, Herrera GM, Van Alstyne KR, Anagnostaras SG. Quantifying the Acoustic Startle Response in Mice Using Standard Digital Video. Front Behav Neurosci. 2020 Jun 3;14:83. doi: 10.3389/fnbeh.2020.00083.
PMID: 32595460; PMCID: PMC7289120.
Laurent JS, Tompkins CL, Cioffredi LA, Wollenburg E, Smith D, Fontaine E. Are we underestimating overweight and obesity prevalence in children? Public Health Nurs. 2020 Jul 20. doi: 10.1111/phn.12773. Epub ahead of print. PMID: 32686151.
Wilson KC, Kaminsky DA, Michaud G, Sharma S, Nici L, Folz RJ, Barjaktarevic I, Bhakta NR, Cheng G, Chupp GL, Cole A, Dixon AE, Finigan JH, Graham B, Hallstrand TS, Haynes J, Hankinson J, MacIntyre N, Mandel J, McCarthy K, McCormack M, Patil SP, Rosenfeld M, Senitko M, Sethi S, Swenson ER, Stanojevic S, Teodorescu M, Weiner DJ, Wiener RS, Powell CA. Restoring Pulmonary and Sleep Services as the COVID-19 Pandemic Lessens: From an Association of Pulmonary, Critical Care, and Sleep Division Directors and American Thoracic Society- coordinated Task Force. Ann Am Thorac Soc. 2020 Jul 14. doi:10.1513/AnnalsATS.202005-514ST. Epub ahead of print. PMID: 32663071.
Friede KA, Infeld MM, Tan RS, Knickerbocker HJ, Myers RA, Dubois LG, Thompson JW, Kaddurah-Daouk R, Ginsburg GS, Ortel TL, Voora D. Influence of Sex on Platelet Reactivity in Response to Aspirin. J Am Heart Assoc. 2020 Jul 21;9(14):e014726. doi: 10.1161/JAHA.119.014726. Epub 2020 Jul 11. PMID: 32654613.
Roth DL, Haley WE, Sheehan OC, Huang J, Rhodes JD, Durda P, Howard VJ, Walston JD, Cushman M. The transition to family caregiving and its effect on biomarkers of inflammation. Proc Natl Acad Sci U S A. 2020 Jul 14;117(28):16258-16263. doi: 10.1073/pnas.2000792117. Epub 2020 Jun 24. PMID:32581123.
Cushman M, Barnes GD, Creager MA, Diaz JA, Henke PK, Machlus KR, Nieman MT, Wolberg AS; American Heart Association Council on Peripheral Vascular Disease, Council on Arteriosclerosis, Thrombosis, and Vascular Biology, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and International Society on Thrombosis and Haemostasis (ISTH). Venous thromboembolism research priorities: A scientific statement from the American Heart Association and the International Society on Thrombosis and Haemostasis. Res Pract Thromb Haemost. 2020 Jul 8;4(5):714-721. doi: 10.1002/rth2.12373. PMID: 32685877; PMCID: PMC7354403.
GRANTS REPORT: UVM SPONSORED PROGRAM ADMINISTRATION
Annual/Monthly Reports for Sponsored Projects
WHAT'S HAPPENING
LCOM Events Calendar | UVM Events Calendar | LCOM Student Activities Calendar
Feedback? Contact Us!
View Archive | Subscribe
Published by the Office of Medical Communications
The Larner College of Medicine
at The University of Vermont
Copyright 2020



